Brain Gut Impact on Mental Health Explained
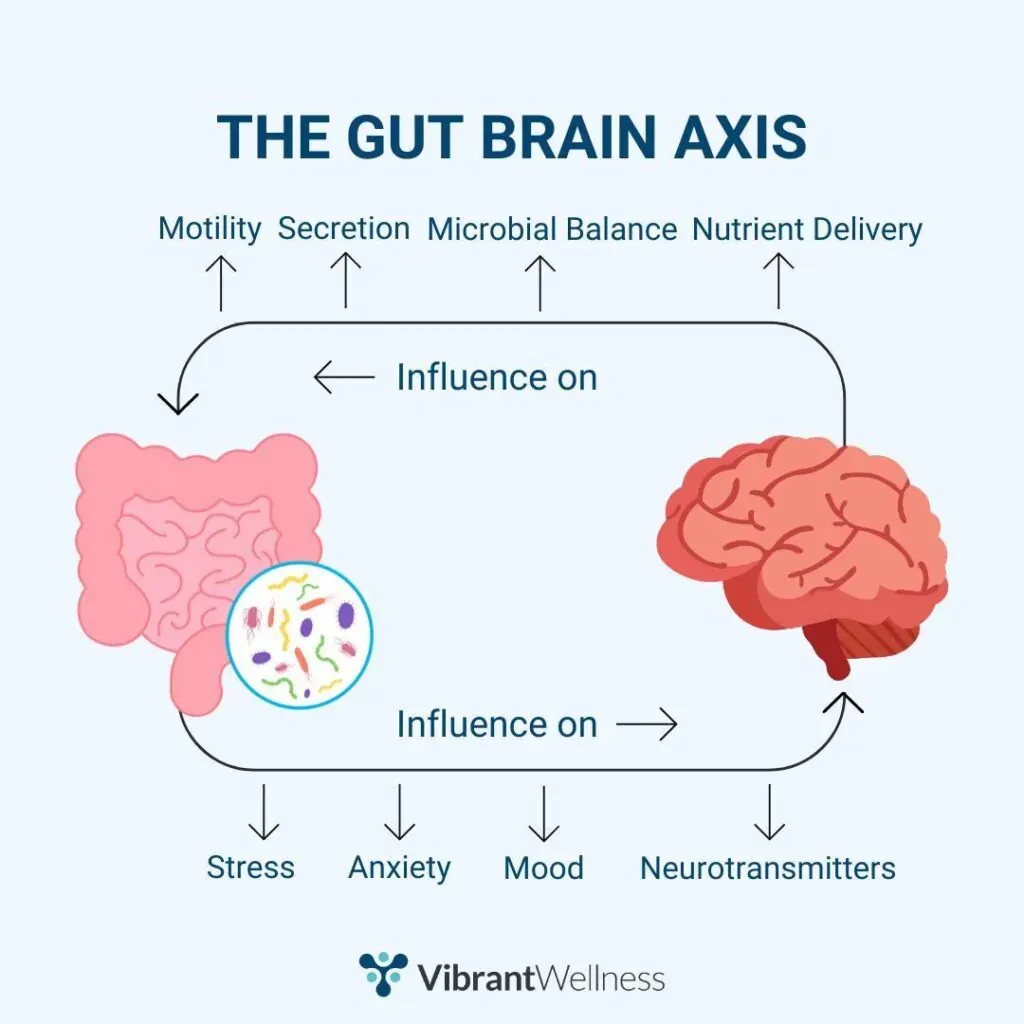
Brain-Gut Impact on Mental Health – The brain-gut connection can greatly determine mental health and the relationship between digestive health and emotional fluctuations. Now known as the gut-brain axis, it’s a bidirectional communication pathway between the central nervous system and the enteric nervous system, which controls gut functions. The gut contains billions of microbes—called the gut microbiota—which secrete neurotransmitters such as serotonin and dopamine that are involved in mood, anxiety, and cognition regulation.

About 90% of serotonin is produced in the gut. Dysbiosis—an imbalance in gut bacteria—has been associated with depression, anxiety, and even neurodevelopmental disorders. Chronic inflammation of the gut inflames the brain, and this reduces gut motility as a stress signal to the brain. This may then aggravate mental health symptoms. Furthermore, mental pressure harms the gut, causing symptoms such as bloating, irritable bowel syndrome (IBS), or indigestion. Thus, promoting gut health with a proper diet that includes prebiotics, probiotics, fiber, and fermented foods may produce emotional regulation and mental clarity. That puts a finer point on the idea that mental health is not all in the head—it is also in the gut and reinforces the need for holistic health.
Brain-Gut Impact on Mental Health
Bidirectional communication along the gut-brain axis
- A two-way communication system, known as the gut-brain axis, which can be mediated through the vagus nerve, hormones, and immune signals, enables the brain to regulate gut function and the gut to influence mood, behavior, and mental health.
Gut Microbiota Influence on Neurotransmitters
- Gut microbiota—the trillions of microbes that reside in the gut—synthesize and modulate the levels of several key neurotransmitters, including serotonin, dopamine, and GABA, all of which influence emotions, anxiety, and depression.
Gut Microbiome and Its Influence on Stress Response
- A balanced gut can attenuate the stress response through the regulation of the HPA axis and the production of the stress hormone cortisol, while a dysregulated gut can enhance stress sensitivity and contribute to mood disorders.
Inflammation and Mental Health
- Also, poor gut health leads to increased intestinal permeability (or leaky gut) and has been shown to result in toxins and inflammatory agents entering the bloodstream and creating chronic inflammation, which has been strongly linked to depression and anxiety.
Role of Probiotics and Prebiotics in Modulating Mental Health
- Dietary inclusion of probiotics (helpful bacteria) and prebiotics (fibers that feed these bacteria) can promote gut health, and available animal and clinical studies indicate these strategies may alleviate anxiety and depressive behaviors in people by restoring a more balanced gut environment and enhancing neurochemical signaling.
The Role of Gut Health in Cognitive Development during Early Life
- The gut microbiota—the microorganisms living in a human’s digestive tract—influences brain and emotional development, and perturbation in early life might predispose individuals to psychiatric illness later on.
The Contribution of Your Diet to Gut-Brain Health
- Fiber, fermented foods, polyphenols, and omega-3 fatty acids—all primary components of the gut-healing diet—provide nourishment to the microbiome, combat inflammation, and promote mental clarity, emotional resiliency, and psychological health.
Brain Gut Connection to Mental Health
The Brain-Gut Connection to Mental Health The relationship between the brain and the gastrointestinal (GI) tract, and specifically the gut, is a complex and bidirectional communication system known as the gut-brain axis. It consists of neural, hormonal, and immune pathways that enable the brain and gut to impact each other in terms of function and health. Here’s an overview:
What It Means:
The gut and the brain are linked, and any change in either will affect the other. Thus, it is no surprise that anxiety, depression, and stress are often accompanied by digestive symptoms and vice versa.
How It Works:
- The vagus nerve is an important messenger relaying signals from the gut to the brain.
- Neurotransmitters (serotonin and GABA, which are responsible for mood and other behaviors) are produced by the gut microbiota (that is, trillions of bacteria that live in our digestive system)
- Gut motility, sensitivity, and inflammation can be affected by stress and emotions, and gut imbalances can affect emotional and cognitive awareness.
Mental Health Implications:
- Chronic inflammation that may have been caused by an unhealthy gut has also been tied to anxiety and depression.
- A healthy gut microbiome promotes clarity of thought, emotional stability, and adaptability to stress.
- Recently, dietary interventions with probiotics and prebiotics have been investigated as adjunct therapies in mental health disorders.
Gut health and mental health are closely linked. Nurturing your gut with your diet, lifestyle, and the way you manage stress is the most important thing you can do for your mood.
Gut Health and Gut-Brain Connection in Allergies
The gut, in all its complex interactions with other systems and barrier tissues, has been discovered to be intricately involved in the development, regulation, and response to all types of allergies, including food allergies, skin reactions, and respiratory allergies. Here is a closer examination of the interaction of these systems:
1. Gut Microbiome’s Role in Allergies
- The gut microbiome, which consists of trillions of bacteria and microbes in the digestive tract, is one of the first lines of defense against allergens.
- A big variety of gut flora, which allows its repertoire of immune cells to know that non-harmful stuff is not the enemy and that the real ones must be dealt with.
- The imbalance in gut bacteria (dysbiosis) excites the immune system and subsequently causes allergies.
2. Gut-Brain Axis and Allergy Symptoms
- The gut–brain axis is a bidirectional communication network between the brain centers responsible for emotion and cognition and the intestinal system.
- The brain controls stress and anxiety responses, both of which can compromise gut barrier function and change microbiome composition, thus increasing reactivity toward allergens.
- This can lead to a very exaggerated allergic reaction, like hives, eczema, or stomach upset.
3. Leaky Gut and Immune Response
- A “leaky gut” (increased intestinal permeability) lets undigested food particles and toxins into your blood.
- This stimulates the immune system, as well as potentially sensitizing the body to allergens and melanoma, encouraging chronic inflammation and allergic disease.
- Some of its most common manifestations are skin rashes, chronic fatigue, bloating, and brain fog.
4. Microbiome Diversity and Immune Tolerance
- More allergies, asthma, eczema, and other complaints develop in children with less contact with a large array of microbes in their infancy.
- Some gut bacteria (such as Bifidobacteria and Lactobacillus) are associated with reduced allergy risk and better gut-brain function.
5. Boosting Gut Health for Allergies
- High-fiber, fermented, prebiotic, and probiotic-rich diets are beneficial to repair the intestinal lining and inhibit inflammation.
- Stress is alleviated by meditation, exercise, and quality sleep, which further improves gut-brain communication and diminishes the allergy response.
That is why your gut microbiome and the gut-brain connection are very important regarding allergens. Gut fortitude bolsters immune tolerance, fights inflammation, and makes it less likely that your body—and your mind—will react to irritants (or allergens) as if they were invading armies.
Q: How Gut Health Affects the Brain
A: The gut affects the brain and vice versa through the gut-brain axis, a bidirectional communication between the gut and the central nervous system. Well, having a healthy gut helps your body produce neurotransmitters such as serotonin, about 90% of which is produced in the gut, and plays a major role in mood, memory, and cognition. Something else is that a healthy gut microbiome lowers systemic inflammation and fortifies the blood-brain barrier, which stops harmful substances from entering the brain. On the other hand, bad gut health can result in more inflammation, intestinal permeability, and even mood disorders like anxiety or depression.
Q: Does Gut Health affect the Brain
Research demonstrates that the health of your gut microbiome can affect mental health, stress response, and neurological health. This can lead to higher amounts of inflammatory cytokines that impair brain function, and an imbalance in the gut microbiome will have an effect opposite to that of a healthy gut when it comes to emotional balance and clarity of thinking, and allow for mood disorders such as depression and anxiety to form.
Q: What vitamin helps Gut Health
A: There are several more essential vitamins for gut health, such as Vitamin D. It assists with the immune system regulation, protects the gut barrier integrity, and encourages the growth of beneficial gut bacteria. Here are a few more types of vitamins that play an important role in gut health:
- Vitamin A: necessary for the maintenance of mucosal surfaces in the gut.
- Vitamin C: This vitamin enhances the immune function and helps to decrease inflammation.
- Vitamin B (particularly B12, B6): Assists digestion and neurotransmitter production.
Q: What vegetables should to avoid for Gut Health
A: Cruciferous vegetables—broccoli, cauliflower, cabbage, Brussels sprouts, etc.—can be an issue for some with gut problems (especially raw). The raffinose and sulfur compounds in these vegetables may contribute to gas, bloating, or digestive discomfort, especially in people with IBS, SIBO, or other sensitive guts. Of course, steaming or preparing them reduces these effects. Additionally, anyone with gut inflammation or autoimmune conditions should omit nightshades (like tomatoes and eggplants) as well.